Best practice use of anthelmintics
Following recent changes to best practice on worm control in horses, Zoetis vet Wendy Talbot navigates the topic to bring practical clarity and help prescribers give the most up-to-date advice to their customers. Wendy is a part of the CANTER core steering group and the best practice guidelines group for Zoetis.
CANTER (Controlling ANTIparasitic resistance in equines responsibly) produced a new set of guidelines last autumn to set out the most sustainable parasite control strategies to address wormer resistance https://canterforhorses.org.uk/prescribers/ The new guidelines have been created as a direct result of detailed discussions between members of the CANTER Guidelines working group which comprises leading veterinary experts and equine professionals. The CANTER guidelines were unveiled in October 2024 at the International Equine Infectious Disease Conference in Deauville, France. It’s important to recognise that some of these guidelines won’t be relevant to some other countries with different climates and different parasite considerations.
BEVA (British Equine Veterinary Association) also produced some new resources in 2024; ProtectMEtoo uses the same principles as CANTER, for vets to ensure that all prescribers are aligned with prescribing advice. BEVA’s resources include a practical toolkit to guide vets through the prescribing process to ensure that the right prescribing decision is made every time.
Both BEVA and CANTER work on the key principles of:
- Risk assessment
- Diagnostic - led
- Annual review
Problem parasites
The most important parasites to affect adult horses in the UK can be divided into two groups: roundworms (nematodes) and tapeworms (cestodes – Anoplocephala spp.). A third group, bots (insects Gasterophilus spp.) also affect horses, however they rarely cause clinical disease.
The main roundworms affecting adult horses are small strongyles (cyathostomins). Large strongyles (Strongylus spp.) can become a problem when worming treatments are infrequent but fortunately, they are not very common in the UK. In foals the most common culprits are large roundworm (Parascaris spp. and intestinal threadworm (Strongyloides westeri).1
1. Risk assessment
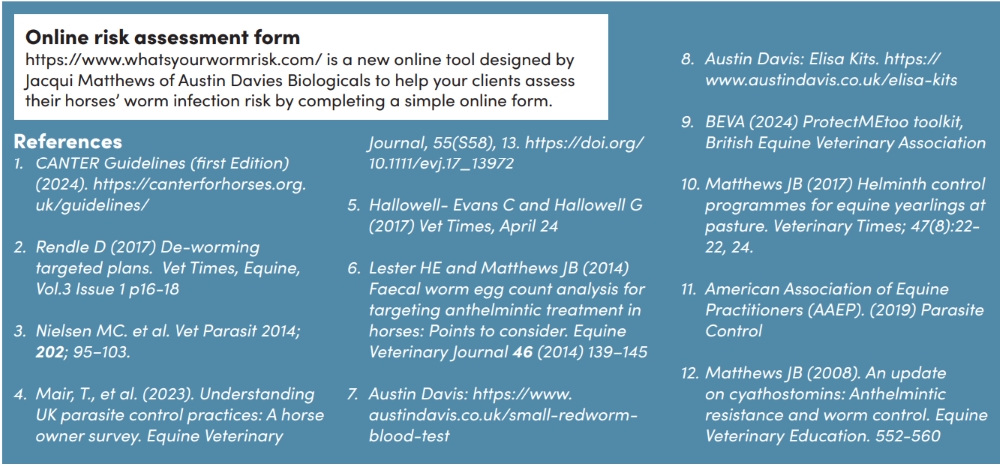
A risk assessment is the cornerstone of every worm control decision, and the CANTER guidelines include a handy table to enable you to evaluate whether the horse is low medium or high risk.
The CANTER acronym is a useful reminder of key elements of a risk assessment: Clinical history, Age profile, Number of horses, Test results, Environment and Risk profile.
2. Diagnostic-led
Faecal Egg Counts (FECs)
FECs measure the number of worm eggs per gram of faeces and give an indication of how much the horse’s worm burden is contributing to pasture contamination. FECs are especially useful to sift out the high shedders from the low shedders in the herd. Usually, around 20% of horses are responsible for 80% of pasture contamination.
By identifying and treating the high shedders we can reduce the amount of shedding onto the pasture and subsequently reduce anthelmintic treatments.
During the spring and summer, FECs can be used to guide appropriate dosing for redworm in adult horses (>3years old). The interval between FECs is variable depending on the horse’s individual circumstances; however, every 2–3 months is a good place to start.2
If an FEC is more than 200 eggs per gram, treatment may be recommended. A result of <50epg (no eggs seen) doesn’t guarantee that there were no eggs in the dung as only a very small sample is studied under the microscope.3
FECs are also used to identify which parasites are affecting the horse and therefore which anthelmintic is best administered if treatment is required. This is particularly important in young foals where the parasite threats change as the foal gets older.1
The third and often overlooked use of FECs is the Faecal Egg Count Reduction Test (FECRT) or ‘resistance test’. FECRTs measure the effectiveness of an anthelmintic administered. The test is easy to perform with a FEC being carried out immediately prior to de-worming with another 2 weeks later. A calculation is performed to determine if there is likely resistance to the administered anthelmintic. The test is most applicable to groups of more than 6 horses grazing together, tested at the same time but may be used to give an indication of dewormer effectiveness in an individual horse. Bear in mind some FEC methods are more precise than others and better suited to perform this test. The CANTER guidelines provide detailed information on the correct sampling and calculation of FECRTs.1
It is recommended to perform FECRTs on any class of wormer used on the premisses in any given year. This will identify any dewormers not fully effective and guide future prescribing decisions to reduce the risk of disease and further development of resistance.
Recent studies show the uptake of FECs amongst horse owners is high4 which is an encouraging development, however, the use of annual FECRTs is still thought to be very low. Educating your customers on the reasons and benefits of FECRTs is a way you can help to impact positive change.
Antibody tests
FECs don’t reveal ‘hidden’ worms such as encysted small redworm or those that are only passed intermittently such as tapeworm, but antibody tests can give an indication by measuring antibody levels.5,6

Antibody tests measure immune cells in the horse’s blood or saliva produced in response to tapeworm or small redworm (blood only). A horse with a high level of tapeworm infection will produce a large number of antibodies, which can be detected in blood or saliva. Depending on the results of a saliva or blood test you will be advised whether a worming medication is required. Because tapeworm antibodies can persist for several months after successful treatment, the results must be interpreted with care and the test cannot be used immediately after a worming medication to check that it has worked. It is recommended to test for tapeworm once or twice a year, depending on risk.
The small redworm test is also an antibody test but is currently only available on blood. It does not distinguish between encysted and other stages of small redworm, but with careful interpretation by a trained professional it can give an indication as to whether encysted stages may be present.7,8,9
3. Annual review
The worming plan should be reviewed at least annually by the prescriber. This will involve ensuring a risk assessment is done, that results of all diagnostic tests and worming treatments used have been recorded and the protocol adjusted as necessary. For example, a horse which is consistently returning high egg counts would raise concerns about the management protocol and possible resistance to anthelmintic classes.
Managing the pasture
Pasture management is an essential component of any worm control plan; less worms on the pasture means less worms are available to infect grazing horses. Several management techniques can significantly reduce the parasite risk in horses and thus reduce the need
for treatment. These include regular poo-picking, ideally every day, but at least twice weekly to prevent worm reinfection, grazing with cattle or sheep who will ‘hoover’ up the worms without being affected, reducing the stocking density in each paddock and creating smaller paddocks so that each field can be alternately grazed and rested. Managing the pasture can reduce reliance on wormers, reducing the drive
for wormer resistance.10
It’s all in the planning
It is important to build a worm control plan for the yard or field as a whole, whilst aiming only to treat each horse based on individual need. This is why individual risk assessments are so important. Not every horse will need treating every time.1

Choosing the right wormer11
By understanding current levels of resistance to major nematode parasites to the three anthelmintic classes we can make the most appropriate prescribing choices. The following world-wide resistance trends have been documented in peer-reviewed studies in managed horse herds.
Benzimidazoles: widespread resistance in cyathostomins reported on multiple continents and early indications of resistance in Parascaris spp. have also been shown.
Pyrimidines: common resistance in cyathostomins reported on multiple continents and early indications of resistance in Parascaris spp.
Macrocyclic lactones: early indications of resistance in cyathostomins were reported in 2019 and widespread resistance in Parascaris spp. More recently, there have been cases of cyathostomins resistance reported to macrocyclic lactones, including in the UK.9
If a risk assessment has been performed and a treatment deemed necessary, it is imperative to choose the right dewormer for the right parasite:
- Small or large redworm
Moxidectin, ivermectin, pyrantel, fenbendazole - Encysted small redworm
Moxidectin or 5-day fenbendazole - Tapeworm
Double dose pyrantel or praziquantel
It’s different for foals
Foals suffer from different parasites at different ages. As a guide, foals should be treated for ascarids at between 2-3 months of age. FECs should be conducted between 4-5 months of age and again at 7-8 months to determine the need for treatment against ascarids and/or cyathostomins.
Foals may also need a strategic autumn/winter treatment for encysted cyathostomins which may replace the treatment at 7-8 months. However, they must be more than 4 months of age for the use of moxidectin.
During the autumn foals should be tested for tapeworm. They must be a minimum of 6.5 months of age if a praziquantel combination product needs to be prescribed.9
Protocols for youngstock
Worm control strategies for youngsters should be based on a risk assessment and diagnostic testing. Youngsters tend to be more susceptible to worms than adult horses because they have had little chance to develop any immunity. FECs should be performed every 2-3 months during the grazing period and ideally faecal egg count reduction tests should also be conducted.
Youngstock don't tend to build up their tapeworm burdens until they start to get to about 6 - 9 months of age. From this time tapeworm ELISA tests should be carried out, ideally on the whole group sharing the field, usually during spring and autumn.
A larvicidal treatment is recommended in the late autumn/winter for youngstock as they are most at risk of larval cyathostominosis. Close monitoring of this age group is crucial to detect any signs of disease, even in those which have been administered a de-wormer.9
Worm control for new horses.
It can be stressful for the new horse when it is presented with a change of environment and change of routine, and this can lead to high shedding and the potential to introduce resistant strains of parasites to the yard.11,12
While a faecal worm egg count can be useful for the new horse it will not show all parasites or all stages. On this basis it is recommended that all new horses should be quarantined on arrival and treated with moxidectin for efficacy against all stages of small and large redworm and praziquantel to treat for tapeworm.11